What the D614G Mutation Means for Covid-19 Spread, Fatality, Treatment, and Vaccine | by Shin Jie Yong | Jul, 2020
medium.com
What the D614G Mutation Means for Covid-19 Spread, Fatality, Treatment, and Vaccine
Real-life implications of the global shift of D614 to G614 variant.
https://medium.com/@shinjieyong?source=post_page-----7dda1c066f0d----------------------
The D614G mutation in SARS-CoV-2 is infamous for its rising dominance worldwide. This mutation changes the amino acid at position 614, from D (aspartic acid) to G (glycine) — so, D-614-G. The initial D614 is now the G614 variant. The question is: What real-life implications do this mutation or G614 variant brings, in terms of transmission, disease severity, treatment, and vaccines?
Is it more transmissible?
In a July study printed in Cell, Dr. Bette Korber, a computational biologist and population geneticist, and colleagues at the Los Alamos National Laboratory analyzed SARS-CoV-2 sequences from 999 patients in the UK. Results showed patients infected with the G614 variant had a higher viral load compared to D614. In human cell cultures in a lab dish, Korber et al. showed that the G614 variant displayed increased infectivity than D614.
Another published study in Cell out of the WHO Collaborating Center in China demonstrated the same. “This dominant [G614] strain could effectively infect the four cell lines tested, being 10-fold more infectious than the original Wuhan-1 strain,” the study authors wrote.
In a research review published in Cell in July too, Nathan D. Grubaugh, an assistant professor of epidemiology of microbial diseases at Yale School of Public Health, and co-workers remarked that such studies suggest, but not prove, increased viral transmissibility. Their review noted that:
- Increased viral shedding or RNA does not reflect viral transmission capacity. Also, most human transmissions occur in the presymptomatic stage, and the above study examined patients in their symptomatic stage.
- Cell culture work does not necessarily translate to humans. Because, as they explained, “These assays don’t account for the effect of other viral or host proteins and the parade of biochemical host-pathogen interactions that must occur to support infection and transmission.”
Is it deadlier?
While Korber et al. found an increased viral load in patients infected with the G614 variant, there was no significant association with disease severity. Two other preprints — one investigating 175 Covid-19 patients from Seattle and the other 88 from Chicago — also did not find any relationship between the G614 variant and clinical outcomes.
Thus, the G614 variant may be more infectious, but not any deadlier than D614. A dead host is a dead-end for viruses after all, so it makes sense for evolution to optimize infectivity while minimizing virulence.
This SARS-CoV-2 Variant Correlates Strongly With Fatality Rates Across Countries
G614 variant evades the host immune response, molecular modeling finds, which could complicate vaccine design.
Before the G614 becomes the dominant global variant; however, researchers at the New York University (NYU) Langone Health found that countries with a higher G614 prevalence had higher case fatality rates (CFRs). Considering the studies discussed above, this finding may no longer hold. The reasons may be that G614 became less virulent, or unadjusted confounding variables. The latter is more likely because, as the study authors admitted, countries may differ in testings, fatality reportings, or social distancing practices.
The G614 variant may be more infectious, but not any deadlier than D614. A dead host is a dead-end for viruses after all, so it makes sense for evolution to optimize infectivity while minimizing virulence.
Is it more challenging to treat?
The three cohort studies presented above found no significant impact of the G614 variant on hospitalization outcomes. Although these studies did not control for treatment types in their analyses, at least the published study of Korber et al. detected that old age and male sex increased the risk of severe Covid-19. Given that fundamental risk factors were present, treatments used in their study should not be any different from other hospitals.
If the G614 variant is indeed more difficult to treat, the case fatality rates (CFRs) will increase over time, given the increasing global prevalence of the G614 variant. But if anything, the CFRs of Covid-19 have either remained the same or decreased — at about 1%.But the efficacy of other drugs that do not rely on inhibiting viral cell entry — e.g., dexamethasone, Medrol, remdesivir, etc. — should remain the same.
The only concern is for therapeutics that inhibit the viral spike protein. Since the G614 variant infects cells more efficiently than D614, cell entry inhibitors might not work so well, Prof. Grubaugh and others cautioned. But the efficacy of other drugs that do not rely on inhibiting the viral spike protein— e.g., dexamethasone, Medrol, remdesivir, etc. — should remain the same.
Is it more challenging for vaccine development?
As a new SARS-CoV-2 variant with distinct biological properties is arising, there were concerns about needing different vaccines for different variants. As scientists at the IMB Cambridge Scientific Center posited back in April: “The highly prevalent [G614] variant in the European population may cause antigenic drift, resulting in vaccine mismatches that offer little protection to that group of patients.”
After three months or so, is it still valid? Unlikely.
Although the D614G mutation happens in the viral spike protein, it does not change the receptor-binding domain (RBD) at the tip of the spike protein (see figure 2). The RBD binds to the ACE2 receptor on human cells; it is also the main target of the immune system. In essence, the D614G mutation alters the spike protein, but not the critical RBD immunogenic part.

However, there is no denying that the D614G mutation produces a minor change in the spike protein structure. This mutation likely enables the spike protein to prime itself in such a way that the RBD can bind the ACE2 receptor more efficiently. This theory is supported by a recent pre-print — of which Dr. Korber is one of the authors — that used structural modeling methods to show that the D614G mutation allows the spike protein to stay in “infection-capable (open) states.”
“Although any of these changes could alter infectivity, it is less likely that it would drastically alter the immunogenicity of RBD epitopes…,” assured Prof. Grubaugh and others. Their review also cited three studies showing that antibodies built from natural D614 and G614 infections can cross-neutralize — meaning that antibodies made against D614 could work for G614, and vice-versa. “The D614G mutation is therefore unlikely to have a major impact on the efficacy of vaccines currently in the pipeline, some of which exclusively target the RBD,” Prof. Grubaugh et al. concluded.
Besides, the study of China WHO showed that the G614 variant remained susceptible to neutralization by antibodies isolated from infected patients. “An amino acid change (D614G) outside the RBD was found to be more infectious, but no evidence of being resistant to neutralizing antibodies has been demonstrated,” they assured.In essence, the D614G mutation alters the spike protein, but not the critical RBD immunogenic part. This mutation likely enables the spike protein to prime itself in such a way that the RBD can bind the ACE2 receptor more efficiently.
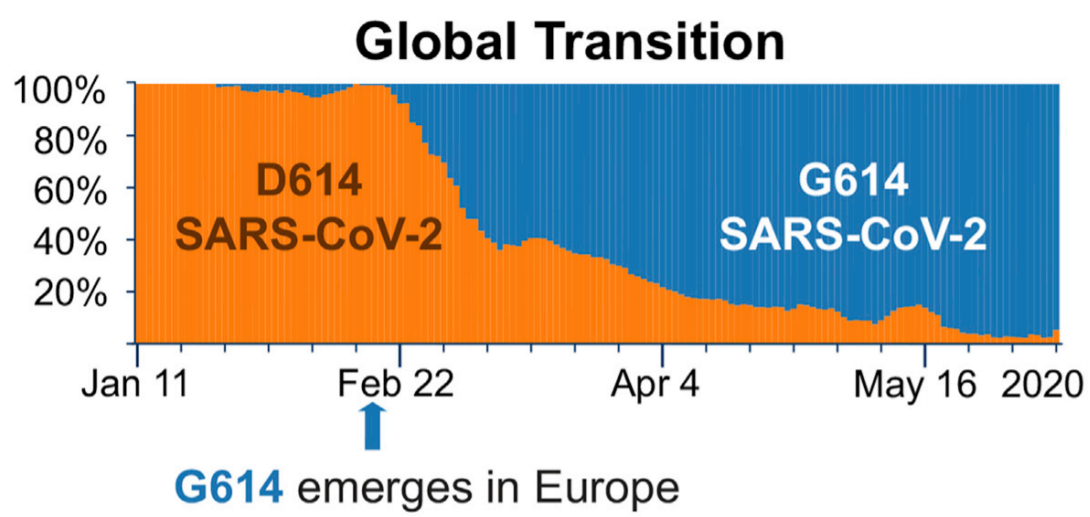
Lastly, we should consider the relative prevalence of G614 and D614 variants. Nearly all circulating SARS-CoV-2 around the world is the G614 variant now (see figure 1). So, there is really no reason for developing two vaccines.
Short Abstract
We are facing the global shift of the SARS-CoV-2 variant — from D614 to G614. The G614 variant is more infectious in laboratory settings; whether it means increased viral spread in humans is unconfirmed. Current evidence says that the G614 variant is not any deadlier than D614. And so, treatment options should not be any more different. Both the D614 and G614 variants should react similarly to vaccines, studies suggest, as the mutation does not change the immunogenic part of the spike protein; that is, the receptor-binding domain (RBD).
