- Joined
- Jul 10, 2008
- Messages
- 65,702
- Points
- 113
Total deaths in the United States show no significant change and even mirror past trends of seasonal illness.
Data is from the CDC which maintains a database of all cause mortality and what the analysis indicates is that deaths have been erroneously classified as Covid deaths when they were actually caused by an existing illness.
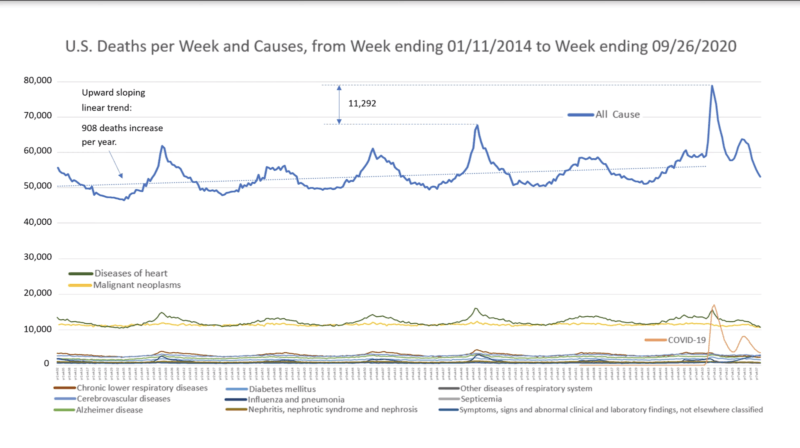
Source: CDC Data, Methodology Included in this Video
According to this graph constructed using data provided by the CDC from the last 6 years, total deaths have remained relatively constant and increases can be explained by various factors such as a larger population. The spikes in deaths in 2020 are consistent with historical trends, only topping 2018 by 11,292 deaths. There have been over 262,000 deaths attributed to Covid-19 in the United States, yet total deaths have not increased in any alarming capacity; they have only mirrored existing trends. In short, according to 6 years of data collected by the CDC, Covid-19 has not led to any significant increase in deaths.
Diving Deeper
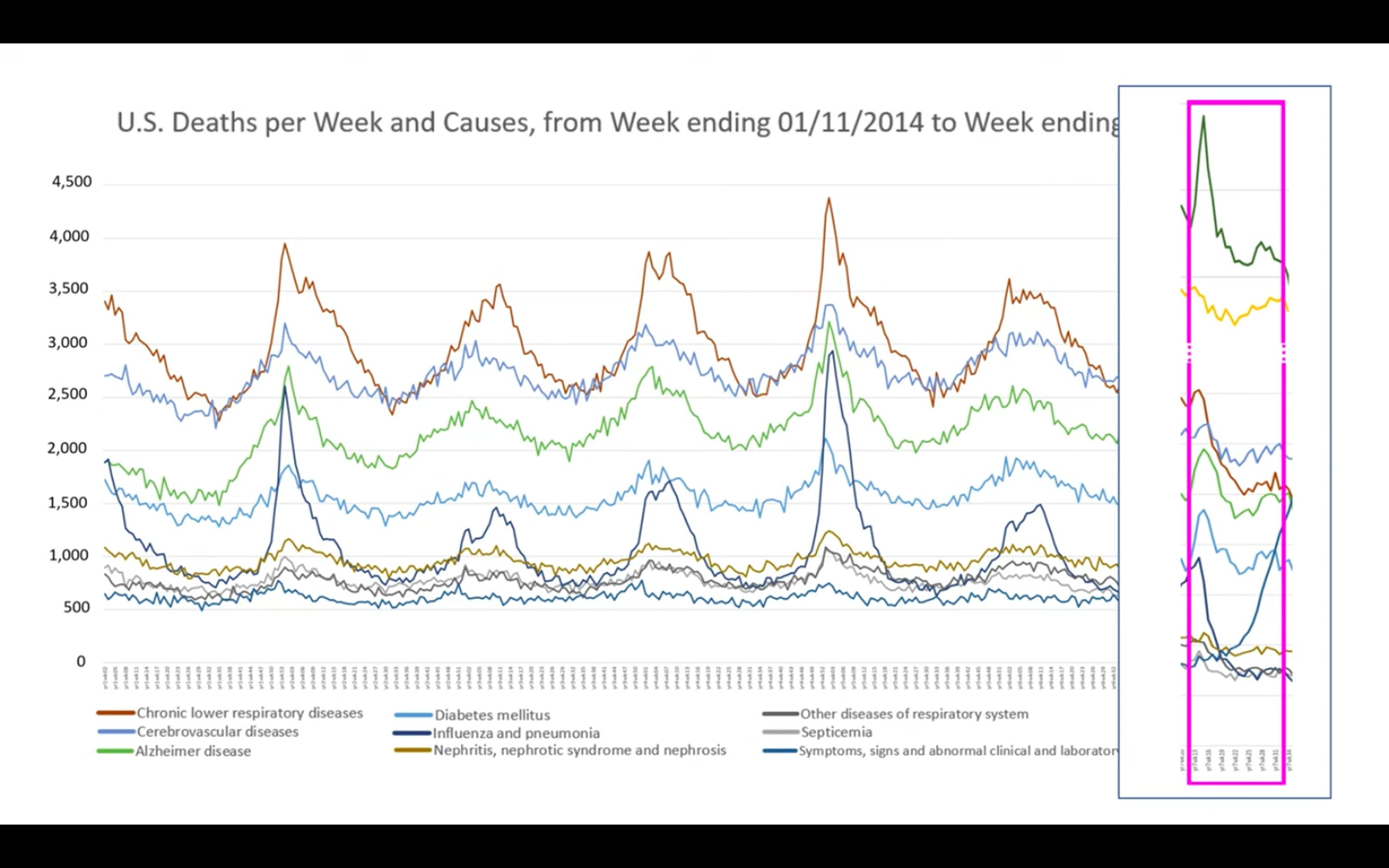
What is even more interesting if not more alarming is that the spike in recorded Covid-19 deaths seen in 2020 has coincided with a proportional decrease in death from other diseases.
Yanni Gu writes
Deaths have remained relatively constant, yet reported deaths due to deadly conditions such as heart disease have fallen while reported Covid deaths have risen. This suggests that the current Covid death count is in some capacity relabeled deaths due to other ailments. According to the graph, reported Covid deaths even overtook heart disease as the main cause of death at one point, which should raise suspicion.
This aligns with many other well-established facts about the virus, such as those with comorbidities are the most at risk. According to the CDC, about 94% of Covid deaths occur with comorbidities. This suggests that it could be possible that a large number of deaths could have been mainly due to more serious ailments such as heart disease but categorized as a Covid-19 death, a far less lethal disease.
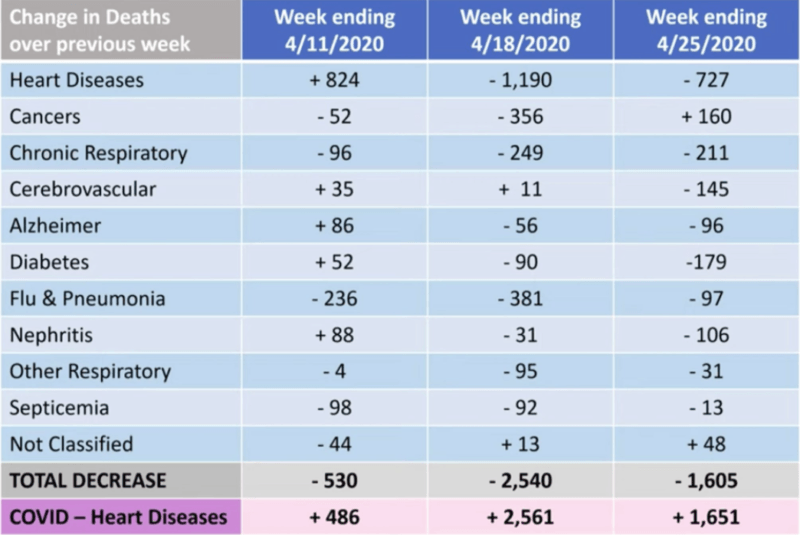 Source: John Hopkins News-Letter, provided by Genevieve Briand
Source: John Hopkins News-Letter, provided by Genevieve Briand
According to this graph provided by the study, deaths labeled under Covid-19 increased while deaths labeled under others decreased. It is important to note that this sample only applies to the month of April as the author notes these were the weeks with the highest reported deaths. Gu writes
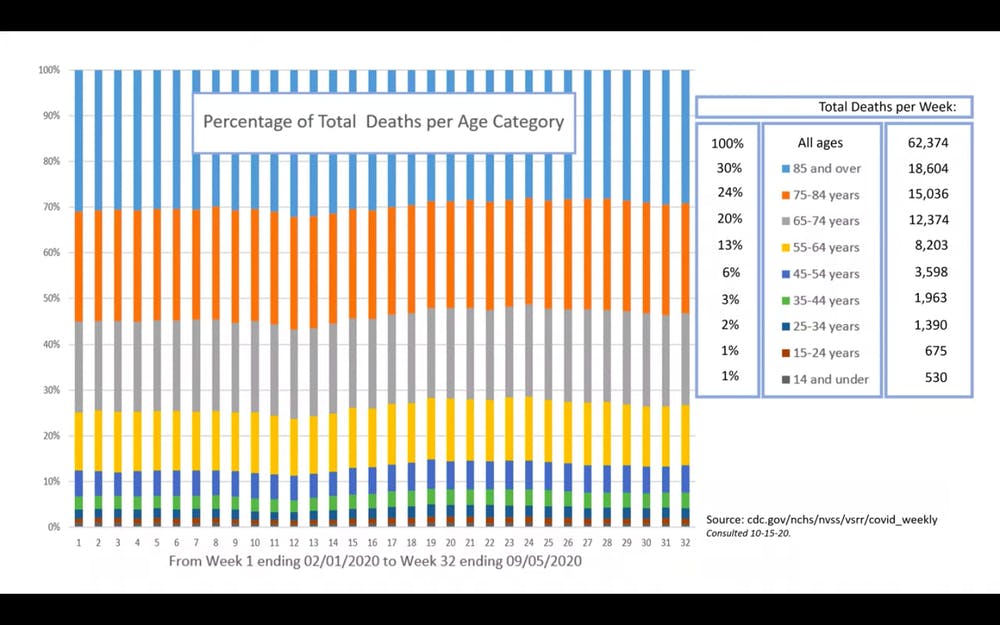
Furthermore, Briand’s research notes that the percentage of death has remained relatively constant through all age groups. Covid death statistics seem to mirror the normal distribution of death amongst age groups, further lending credence to the argument that many Covid deaths are recategorized deaths.
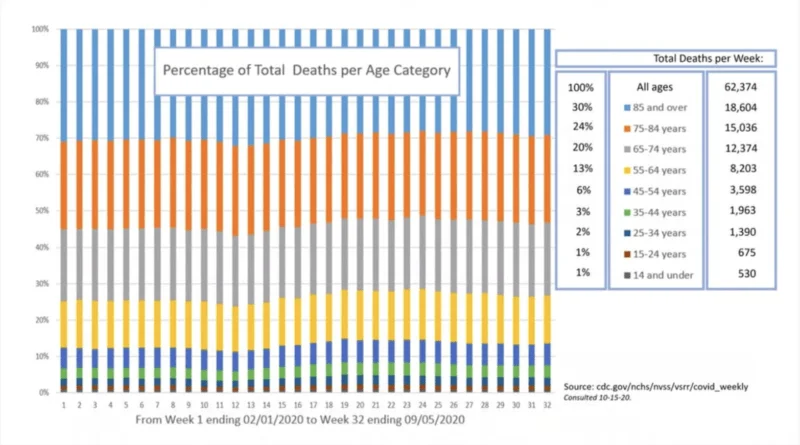
Briand provides this graph constructed from CDC data that shows that deaths amongst various age groups have remained relatively constant.
By simply looking at the raw data presented by the CDC Gu writes that
Briand and likely many others suppose that the extreme emphasis on Covid-19 has led to the unintended classification of the disease as the cause of death. She further stresses that although this data challenges the idea that Covid is an unprecedented and lethal disease, we should still be concerned with mitigating death in general.
However, it is clear that this significant accounting error regarding Covid deaths, if true, is not productive. It has caused mass hysteria and misinformed public policy. Closing down communities to fight a virus that according to the data, has had no significant contribution to total deaths, reduces our overall capacity to build a healthy society.
Lockdowns have resulted in severe damage to our capacity to improve the general health of society. From the catastrophic economic damage that lowers the standard of living for everyone to surgeries being deemed “unessential,” our current policies are not helping in preventing deaths in general; they are likely leading to more. Suicides and substance abuse are up, mental and physical health are down, all due to lockdowns.
The late Dr. Donald Henderson, who led the eradication of smallpox, noted in 2006 that
The hysteria over Covid-19 has likely led to the alleged accounting error noted in Briand’s study, the reclassification of expected deaths from all causes into Covid deaths. That accounting error has likely led to a number of policy decisions that have drastically crippled our ability to support the general welfare of society, economically, socially, and spiritually. Going forward these findings should give us pause and reconsideration over the threat Covid-19 actually poses and realize how much avoidable damage we have done to ourselves as a result.
Data is from the CDC which maintains a database of all cause mortality and what the analysis indicates is that deaths have been erroneously classified as Covid deaths when they were actually caused by an existing illness.
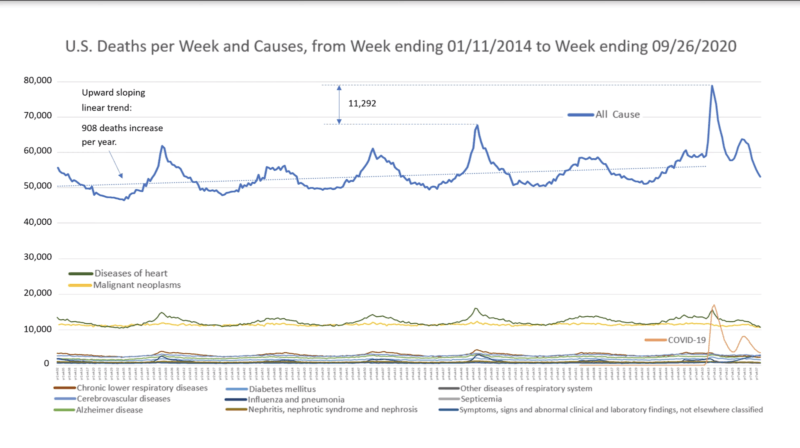
Source: CDC Data, Methodology Included in this Video
According to this graph constructed using data provided by the CDC from the last 6 years, total deaths have remained relatively constant and increases can be explained by various factors such as a larger population. The spikes in deaths in 2020 are consistent with historical trends, only topping 2018 by 11,292 deaths. There have been over 262,000 deaths attributed to Covid-19 in the United States, yet total deaths have not increased in any alarming capacity; they have only mirrored existing trends. In short, according to 6 years of data collected by the CDC, Covid-19 has not led to any significant increase in deaths.
Diving Deeper
What is even more interesting if not more alarming is that the spike in recorded Covid-19 deaths seen in 2020 has coincided with a proportional decrease in death from other diseases.
Yanni Gu writes
“This suggests, according to Briand, that the COVID-19 death toll is misleading. Briand believes that deaths due to heart diseases, respiratory diseases, influenza and pneumonia may instead be recategorized as being due to COVID-19.”
Deaths have remained relatively constant, yet reported deaths due to deadly conditions such as heart disease have fallen while reported Covid deaths have risen. This suggests that the current Covid death count is in some capacity relabeled deaths due to other ailments. According to the graph, reported Covid deaths even overtook heart disease as the main cause of death at one point, which should raise suspicion.
This aligns with many other well-established facts about the virus, such as those with comorbidities are the most at risk. According to the CDC, about 94% of Covid deaths occur with comorbidities. This suggests that it could be possible that a large number of deaths could have been mainly due to more serious ailments such as heart disease but categorized as a Covid-19 death, a far less lethal disease.
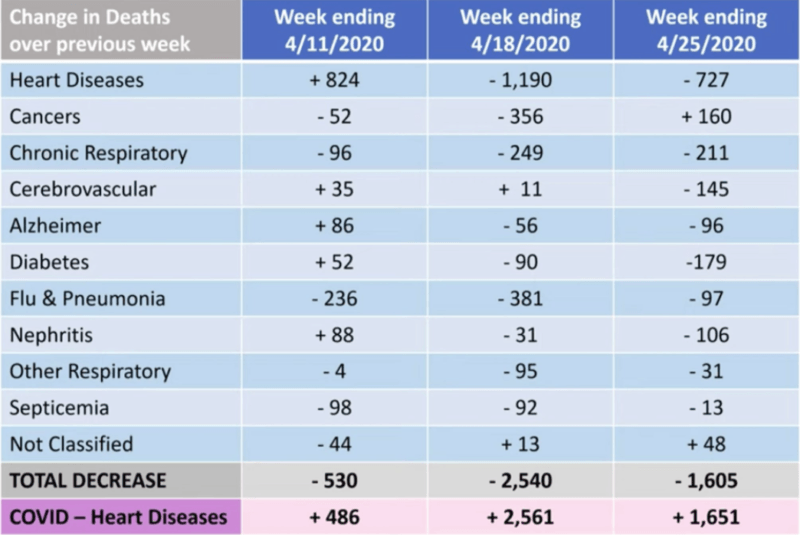
According to this graph provided by the study, deaths labeled under Covid-19 increased while deaths labeled under others decreased. It is important to note that this sample only applies to the month of April as the author notes these were the weeks with the highest reported deaths. Gu writes
“The CDC classified all deaths that are related to COVID-19 simply as COVID-19 deaths. Even patients dying from other underlying diseases but are infected with COVID-19 count as COVID-19 deaths. This is likely the main explanation as to why COVID-19 deaths drastically increased while deaths by all other diseases experienced a significant decrease…
“If [the COVID-19 death toll] was not misleading at all, what we should have observed is an increased number of heart attacks and increased COVID-19 numbers. But a decreased number of heart attacks and all the other death causes doesn’t give us a choice but to point to some misclassification,” Briand replied.”
Furthermore, Briand’s research notes that the percentage of death has remained relatively constant through all age groups. Covid death statistics seem to mirror the normal distribution of death amongst age groups, further lending credence to the argument that many Covid deaths are recategorized deaths.
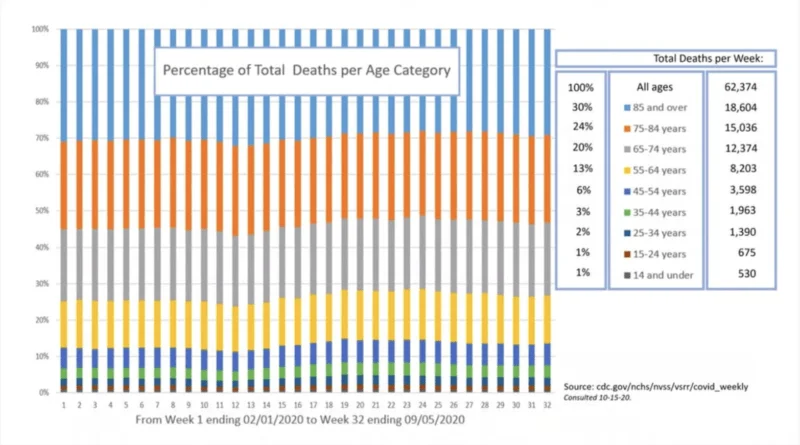
Briand provides this graph constructed from CDC data that shows that deaths amongst various age groups have remained relatively constant.
By simply looking at the raw data presented by the CDC Gu writes that
What Do We Do With This Information?“All of this points to no evidence that COVID-19 created any excess deaths. Total death numbers are not above normal death numbers. We found no evidence to the contrary,” Briand concluded.
Briand and likely many others suppose that the extreme emphasis on Covid-19 has led to the unintended classification of the disease as the cause of death. She further stresses that although this data challenges the idea that Covid is an unprecedented and lethal disease, we should still be concerned with mitigating death in general.
However, it is clear that this significant accounting error regarding Covid deaths, if true, is not productive. It has caused mass hysteria and misinformed public policy. Closing down communities to fight a virus that according to the data, has had no significant contribution to total deaths, reduces our overall capacity to build a healthy society.
Lockdowns have resulted in severe damage to our capacity to improve the general health of society. From the catastrophic economic damage that lowers the standard of living for everyone to surgeries being deemed “unessential,” our current policies are not helping in preventing deaths in general; they are likely leading to more. Suicides and substance abuse are up, mental and physical health are down, all due to lockdowns.
The late Dr. Donald Henderson, who led the eradication of smallpox, noted in 2006 that
“Experience has shown that communities faced with epidemics or other adverse events respond best and with the least anxiety when the normal social functioning of the community is least disrupted.”
The hysteria over Covid-19 has likely led to the alleged accounting error noted in Briand’s study, the reclassification of expected deaths from all causes into Covid deaths. That accounting error has likely led to a number of policy decisions that have drastically crippled our ability to support the general welfare of society, economically, socially, and spiritually. Going forward these findings should give us pause and reconsideration over the threat Covid-19 actually poses and realize how much avoidable damage we have done to ourselves as a result.