- Joined
- Feb 26, 2019
- Messages
- 12,449
- Points
- 113
my.clevelandclinic.org
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
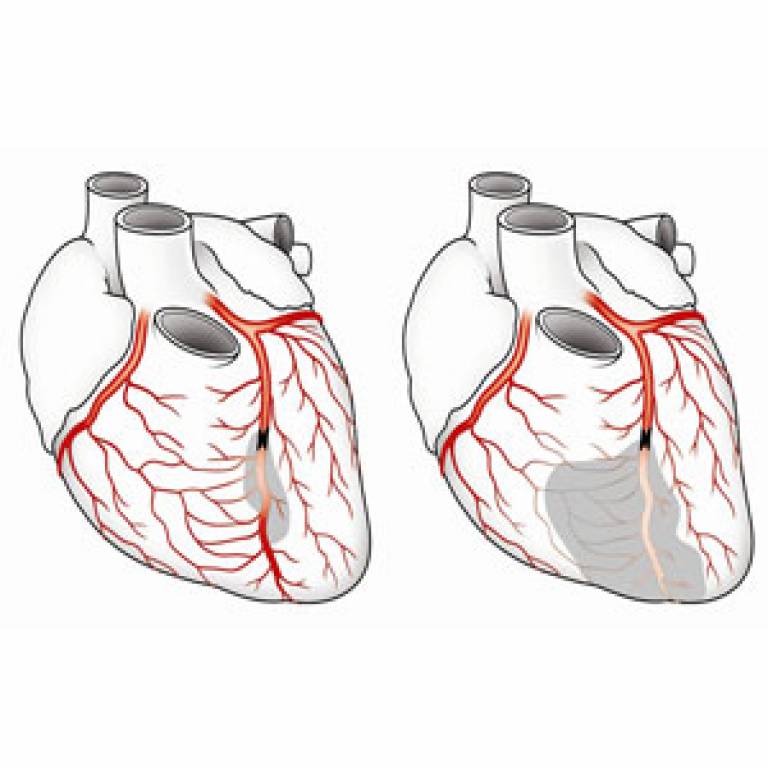
Angiogenesis may happen as a main blood vessel slowly becomes blocked. Your body senses the reduced blood flow and calls other blood vessels into action. Regular aerobic exercise, such as running, may also encourage new collateral blood vessels to form.
Collateral blood vessels cannot always prevent ischemia (lack of blood supply) from these health conditions. Collateral vessels must expand quickly enough to take over blood flow before the blood supply is completely blocked. These health conditions always require treatment, even in people who have good collateral blood vessels.
But as you get older, your collateral blood vessels gradually shrink. This process, called rarefaction, is more likely to happen in people who have cardiovascular disease. When your collateral blood vessels shrink, they are less likely to work, which can lead to symptoms when blood flow becomes blocked in your main blood vessels.
Collateral circulation is your body’s way of working around a blockage in blood flow. It’s not a foolproof way to prevent damage from conditions like stroke and PAD, or to prevent a heart attack or stroke. However, it can be helpful and possibly lifesaving in some cases.
Researchers are continuing to study collateral circulation and the possibility of creating and using artificial collateral veins. This could expand the body’s natural ability to overcome a variety of conditions that obstruct blood flow.
What is collateral circulation?
Collateral circulation is alternate or “backup” blood vessels in your body that can take over when another artery or vein becomes blocked or damaged. Your collateral circulation provides alternative routes for blood flow.Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
How does collateral circulation work?
Collateral blood vessels connect to your main blood vessels and remain small and unused until you need them. Other collateral vessels develop throughout life in a process called angiogenesis (the formation of new blood vessels).Angiogenesis may happen as a main blood vessel slowly becomes blocked. Your body senses the reduced blood flow and calls other blood vessels into action. Regular aerobic exercise, such as running, may also encourage new collateral blood vessels to form.
How common is collateral circulation?
Usually, people are born with some collateral blood vessels, but the number and size are different for each person. Collateral blood vessels can be:- Arteries, larger blood vessels that carry blood away from your heart.
- Capillaries, tiny blood vessels that help transport oxygen and nutrients.
- Veins, carry blood back to your heart.
What health conditions are related to collateral circulation?
Your collateral circulation may take over if you have health conditions that restrict blood flow, such as:Collateral blood vessels cannot always prevent ischemia (lack of blood supply) from these health conditions. Collateral vessels must expand quickly enough to take over blood flow before the blood supply is completely blocked. These health conditions always require treatment, even in people who have good collateral blood vessels.
How long does collateral circulation last?
When your collateral circulation takes over, smaller blood vessels must get larger to accommodate the increased blood flow. The enlarged collateral vessels may continue to accommodate your normal blood flow for months or years.But as you get older, your collateral blood vessels gradually shrink. This process, called rarefaction, is more likely to happen in people who have cardiovascular disease. When your collateral blood vessels shrink, they are less likely to work, which can lead to symptoms when blood flow becomes blocked in your main blood vessels.
Where does collateral circulation occur?
Various parts of your body can have collateral circulation, including your:- Abdomen.
- Arms.
- Brain.
- Feet and legs.
- Heart.
- Lungs.
Collateral circulation is your body’s way of working around a blockage in blood flow. It’s not a foolproof way to prevent damage from conditions like stroke and PAD, or to prevent a heart attack or stroke. However, it can be helpful and possibly lifesaving in some cases.
Researchers are continuing to study collateral circulation and the possibility of creating and using artificial collateral veins. This could expand the body’s natural ability to overcome a variety of conditions that obstruct blood flow.