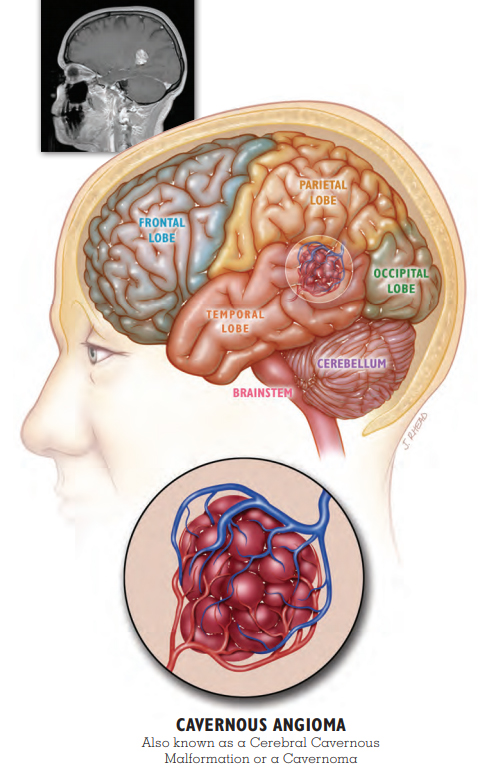
1) What is Cavernous Malformation?
Cavernous malformations are also known as cavernous angioma, CCM, and cavernoma. They are made of abnormal blood vessels. They are not cancerous. Cavernous malformations are made of the smallest blood vessels, called capillaries. They resemble mulberries and have very thin walls compared with other blood vessels. Blood moves through them very slowly. The thin vessel walls can be leaky, allowing blood into the surrounding brain or spinal cord tissue. We believe about one in every 500 people has a cavernous malformation, but most people never have symptoms. Of the people who have a cavernous malformation, we believe many will never have a symptomatic hemorrhage.
The rarest place for a symptomatic cavernous malformation is in the spinal cord. A spinal cord cavernous malformation is not the same as a spinal hemangioma, which is located in the vertebra (bone). Cavernous malformations may also occur in the area of the brain called the brainstem. Spinal cord and brainstem cavernous malformations can cause more severe symptoms when they hemorrhage.
Sporadic Cavernous Malformation with Seizure
Stacie awakened in the middle of the night, just like many other nights. Only this time, as she tried to walk across the room, she became unsteady and fell into the wall. The dizziness happened again the next morning. A 36-year-old mother of four, Stacie sought medical help, but after numerous tests, the doctors were unable to provide her with a diagnosis.
One evening a year later, Stacie experienced what she later would learn was a series of partial complex seizures that included involuntary movement, a loss of awareness, and difficulty speaking. Her husband rushed her to the local hospital where a CT scan revealed an unidentified mass deep in her right temporal lobe. Stacie transferred to a larger hospital with more advanced diagnostic capabilities where she received an MRI.
Her brain mass was diagnosed as a cavernous malformation (cavernous angioma, cavernoma), and she was discharged on anti-seizure medication. Despite this, the seizures continued, and she sought a surgical consultation. The doctors informed her that removing her lesion would be difficult because of its deep location, and surgery could cause additional harm. Stacie needed to accept her new normal.
It has been a year since her diagnosis. After trying a few different anti-seizure medications to find the best fit, Stacie’s seizures are now under control. She says she has learned to leave her high heels in the closet because she still experiences dizziness. Sometimes she has trouble finding the right words. “It’s like playing charades with my kids,” laughs Stacie. “Eventually they figure out what I mean.” She is happy to be driving again and to be able to take care of her family.
Says Stacie, “My brain hemorrhage changed my life, but I know there’s a reason. I will use it as a strength and not a weakness.”
2) WHAT IS AN INCIDENTAL CAVERNOUS malformation?
Your doctor may have discovered your cavernous malformation (cavernous angioma, cavernoma) when you had brain or spinal imaging for a reason not related to your cavernous malformation. For example, you may have received a CT scan or an MRI after a car accident or concussion. In this case, doctors will call your cavernous malformation an
incidental finding. Research has shown that incidental cavernous malformations that have not had a previous hemorrhage have a very small chance of ever becoming problematic. While you may want to follow the precautions listed in the
Hemorrhage section of this booklet, you may not need repeat imaging unless instructed by your doctor or you develop symptoms. However, many doctors and patients choose to have imaging, typically with MRI, to monitor the lesion. For example, your doctor may order imaging during pregnancy, after medication changes, if another illness is diagnosed, or at times of dramatic lifestyle change, which can include extreme or unusual exercise.
3) WHO MIGHT BE INVOLVED IN MY CARE?
- NEUROLOGIST – manages symptoms like seizure and pain
- NEUROSURGEON – evaluates for surgery
- REHABILITATION SPECIALISTS – improve functioning after brain event
- ORTHOPEDIST – monitors spine in CCM3 patients (see Genetics)
- NEURO-OPHTHALMOLOGIST – cares for brain-related vision problems
- GENETICIST – evaluates for the hereditary form of the illness
- DERMATOLOGIST – cares for vascular skin lesions in hereditary illness
4) WHAT CAUSES MULTIPLE CAVERNOUS malformations?
Some people have more than one cavernous malformation (cavernous angioma, cavernoma). This can happen for several reasons:
- Most commonly, people with more than one cavernous malformation have a hereditary form of the illness. People with the genetic form of the illness typically develop additional cavernous malformations over time.
- Some people may have a second kind of abnormal blood vessel called a developmental venous anomaly (DVA). Your doctor might also call this a venous malformation or venous angioma. This dilated blood vessel only rarely causes symptoms on its own. However, it may create conditions that make it more likely for cavernous malformations to form. This is not hereditary.
- Brain or spinal radiation for cancer treatment can cause cavernous malformations to form many years later. In people with the hereditary form, radiosurgery to treat a cavernous malformation may also cause more lesions to form. You can find more information about radiosurgery in the section on Other Treatments.
5) WHAT IS SPORADIC CAVERNOUS Malformation (Cavernous angioma, cavernoma)?
Sporadic cavernous malformation means that you are the only one in your family to have a cavernous malformation, and you do not have a genetic mutation that would cause your children to inherit the illness. Usually, individuals with the sporadic form of the illness have just one cavernous malformation with no other visible blood vessel abnormalities or medical history to explain the lesion.
Sometimes, individuals have a different kind of blood vessel abnormality called a
developmental venous anomaly (DVA) or they have a history of brain radiation for cancer. A DVA or brain radiation can lead to the development of one or more cavernous malformations (see
What Causes Multiple Cavernous Malformation? above). To be certain you have the sporadic form of the illness, you will need to have an MRI with some special images called susceptibility-weighted imaging or SWI. Ask your doctor if this was part of your original MRI. See Stacie and Vern’s Patient Stories to learn more about sporadic cavernous malformation with and without a DVA.
6) WHAT IS A BLEED OR HEMORRHAGE?
All cavernous malformations (cavernous malformations, cavernomas) have some chronic oozing of blood in the area of the lesion. This is what gives their typical appearance on MRI. Oozing is different from the more significant hemorrhage or bleed. A
hemorrhage is new bleeding in the cavernous malformation and is often associated with new symptoms. Symptomatic hemorrhage is the most serious complication of cavernous malformation and is the most common reason for surgery. The hemorrhage may cause new symptoms or an increase in symptoms. The specific symptoms a person experiences will depend on the location and size of the cavernous malformation and the amount of blood that has leaked outside the lesion. Eventually, the blood breaks down leaving behind an iron deposit called hemosiderin.
Most lesions never hemorrhage. However, once a cavernous malformation has had one hemorrhage, it is at a significantly greater risk of bleeding again. In the first five years after a hemorrhage, the risk of another hemorrhage in a cavernous malformation that is not in the brainstem is 17-20% (1 in 5 lesions will have a second hemorrhage). The risk of a second hemorrhage in brainstem cavernous malformations is greater at 30% (1 in 3 lesions will have a second hemorrhage). Most of these second hemorrhages will take place in the first two years after the original hemorrhage. Fortunately, five years after a hemorrhage, the risk of another hemorrhage gradually returns to a rate that is similar to the risk from a lesion that has never bled.