Doctor suspended 3 years, fined $25,000 for overprescribing cough mixtures containing codeine

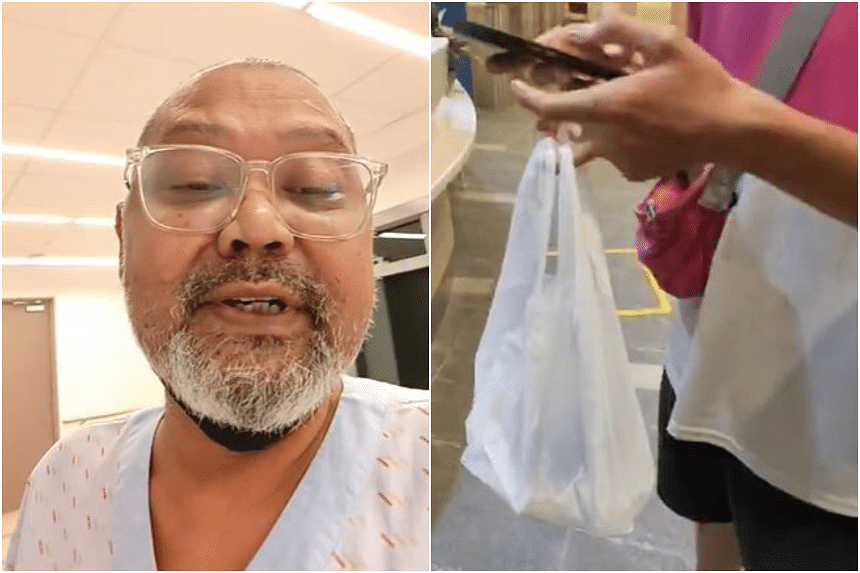
Dr Andrew Tang Yen Ho had prescribed 270ml of cough mixture to each of the 10 patients. PHOTO: ST FILE

Salma Khalik
Senior Health Correspondent
MAY 4, 2020
SINGAPORE - A doctor has been suspended for three years and fined $25,000 for overprescribing cough mixtures containing codeine to 10 patients.
This is the second such infringement for Dr Andrew Tang Yen Ho of Tang Medical & Surgery at Block 8 Jalan Batu.
In May 2013, the Singapore Medical Council (SMC) suspended him for six months over a similar offence.
Dr Tang, who was also fined $10,000, gave an undertaking then that he would not re-offend.
But in 2015, the Ministry of Health (MOH) audited the medical records at his clinic and was concerned about his prescription of cough mixtures containing codeine.
Codeine is an opiate, and excessive use could lead to addiction and abuse.
The ministry then sent a letter to the SMC to investigate the matter.
But the doctor did not respond to any of SMC's queries, which forced the professional watchdog to serve him a notice of inquiry in February last year.
In spite of multiple attempts by the SMC to contact him, which included a hand-delivered letter that was accepted by a woman claiming to be his mother, Dr Tang did not attend the hearing and subsequent judgment and sentencing.
He also did not appoint anyone to represent him.
The SMC had checked with the Immigration and Checkpoints Authority to ascertain that he was in Singapore on the relevant dates.
Dr Tang faced 30 charges in all.
They involved three offences against each of the 10 patients: inappropriate prescription of the cough mixture, failure to exercise competent and due care of his patients, and failure to keep proper medical records.
The disciplinary tribunal (DT) found him guilty of inappropriate prescription, but acquitted him of the other charges.
The tribunal found that Dr Tang had prescribed 270ml of cough mixture containing codeine to each of the 10 patients on multiple occasions.
This was more than the 240 ml limit per patient per visit, as advised by the MOH.
In its written judgment published on Monday (May 4), the tribunal said: "The number of times the respondent 'overprescribed' the quantity of cough mixture containing codeine for each patient ranged from four to 21 times."
It added that he had also prescribed the cough mixture within four days of the previous visit on four occasions, involving four of the patients.
The SMC's lawyer had asked for a 36-month suspension for each of the three most serious charges, to run consecutively.
In other words, a total suspension of nine years.
As the tribunal is only empowered to impose a maximum suspension of three years, the counsel then asked for the doctor to be struck off the register to reflect the severity of the offence.
However, the tribunal did not agree that "just because the DT cannot impose any heavier suspension sanction than three years, a striking off is the only other option".
This, it said, would violate the principle as "a striking off would be a crushing sentence on the respondent in relation to the level of misconduct".
This was partly because, while there was potential harm, there had been no real harm done to any of the 10 patients.
It decided that the just penalty is the maximum suspension of three years, and a fine of $25,000.
The doctor also has to pay the cost of the proceeding, including SMC's legal costs.
The tribunal dismissed the other 20 charges.
It said that none of the 10 patients were given solely cough mixture containing codeine.
They were also given other medication to treat their various problems, and hence Dr Tang's treatment "was not unacceptable".
It added that his medical record-keeping, though "not up to standard", was "not inadequate".